Anterior Uveitis – Red and/or Light Sensitive Eye(s)
Anterior uveitis needs to be monitored on a regular basis, but with proper treatment, it can be put into remission
I often like to think of our eyes as windows to the soul. But more appropriately, the eyes are more like a window into systemic health.
I’ve talked in the past about diabetes, hypertension, and high cholesterol, and how those diseases affect the eyes. Many times, younger patients diagnosed with these particular diseases get tipped off during a routine eye exam.
When the eye(s) starts to get red, a whole host of issues can be assumed. However, a patient really won’t know what’s going on until he/she consults his/her eye doctor.
Most patients assume abnormal redness is irritation or “pink eye”. But sometimes it can be a viral or bacterial infection. Sometimes it can be an allergic reaction. Sometimes it can be much worse.
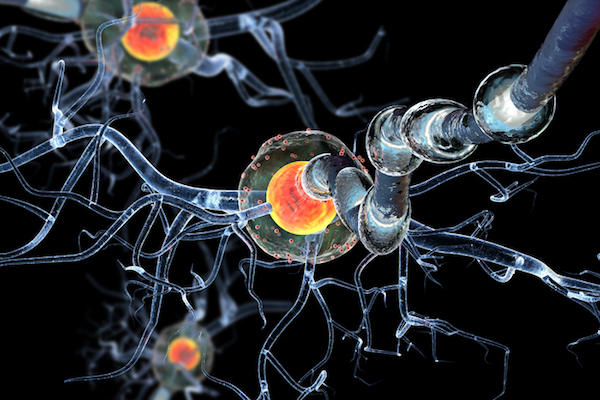
One particular condition which causes redness of the eye(s) is called anterior uveitis. This can be best described as a breakdown of the blood aqueous barrier.
In simpler terms, anterior uveitis occurs when inflammatory cells move to the front part of the eye. It can effect one or both eyes, and it can occur one time or several times over many years.
Signs & Symptoms:
On a daily basis, I’m fortunate to meet several amazing people as my patients. One of my absolute favorite patients is a contact lens wearer who once came to my office with very red and light sensitive eyes. Being somewhat of a tough guy, he thought he’d just grit through the pain, but it eventually became too much. I told him, “I’m thankful the pain was unbearable because we caught your uveitis before significant damage to the eyes had occurred.”
You may be experiencing anterior uveitis if you’re dealing with any of the following symptoms:
- Red eye(s)
- Painful eye(s) – usually a 3/5 on a pain scale
- Light sensitive eye(s)
- Blurry vision
It’s worth it to mention that patient’s who have anterior uveitis often go undiagnosed. This is because he/she thinks it’s just “pink eye” and it’ll go away sooner rather than later. This can be a dangerous situation because untreated anterior uveitis can lead to more severe ocular problems.
Half of anterior uveitis cases occur from an underlying cause. The other half of the time, it’s idiopathic, which means we don’t know the actual cause. An underlying cause of uveitis can be one of the following systemic diseases:
- Tuberculosis
- Syphilis
- Herpes virus
- Ulcerative Colitis
- Crohn’s Disease
- Reactive Arthritis
- Psoriatic Arthritis
- and more
If any of these diseases are found to be the underlying cause of anterior uveitis, your eye doctor will refer you to the appropriate specialist. It’ll most likely be a rheumatologist, an internal medicine physician, an infectious disease specialist, or a gastroenterologist (depending on what the lab work reveals).
Treatment Options:
Your eye doctor will typically use one of the following treatments for anterior uveitis:
- Eye drops
- Injections
- Oral medications
In my opinion, anterior uveitis is best treated with a topical steroid and a cycloplegic eye drop to help with pain. This combination will ease the pain quickly, but make sure to follow all instructions because the topical steroids will need to be tapered slowly prior to being stopped altogether.
During this time, your eye doctor will also monitor eye pressure. This is because steroid use could cause eye pressure to rise, which could potentially lead to glaucoma.
For tougher cases, stronger medication can be given (like oral methotrexate for example).
Live in Your OcularPrime:
If you find yourself in a painful/red eye situation, make sure to check in with your eye doctor right away. A correct diagnosis and proper treatment will be initiated as soon as possible.
Anterior uveitis can reoccur and needs to be monitored on a regular basis. But with proper treatment, it can be put into remission.